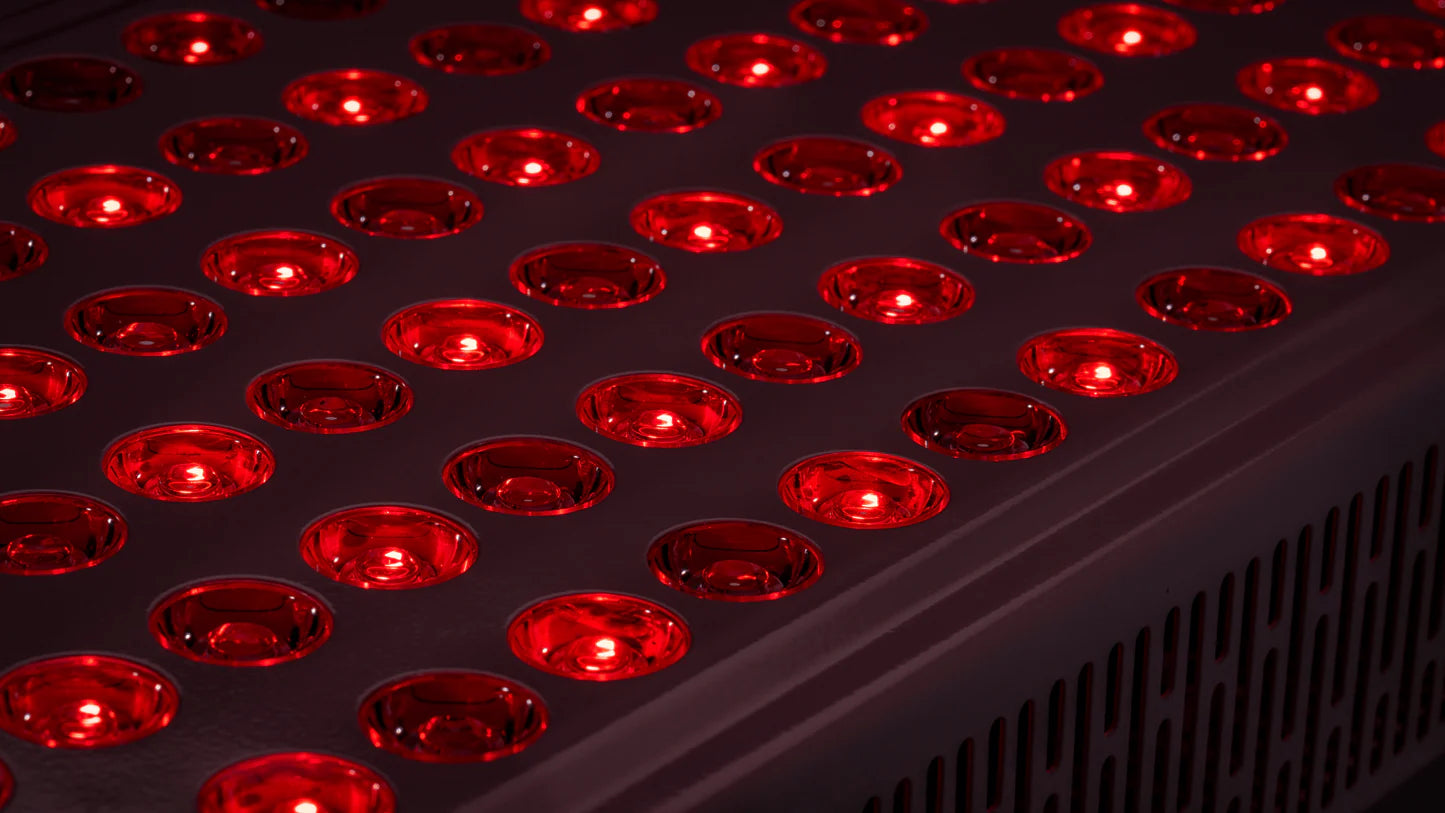
LLLT & Dual-Wavelength LLLT?
LLLT is a photobiomodulation therapy that uses precise wavelengths of light to stimulate cellular energy production and repair. Originally developed by NASA for medical research, LLLT has now been successfully adapted to manage dry eye disease.
by irradiating the eyelids and Meibomian glands with LEDs at 635nm (visible red light) and 850nm (near-infrared light), DWV™ LLLT stimulates ocular metabolism through PBM (photobiomodulation), harnessing biological regulatory effects to enhance eye health.
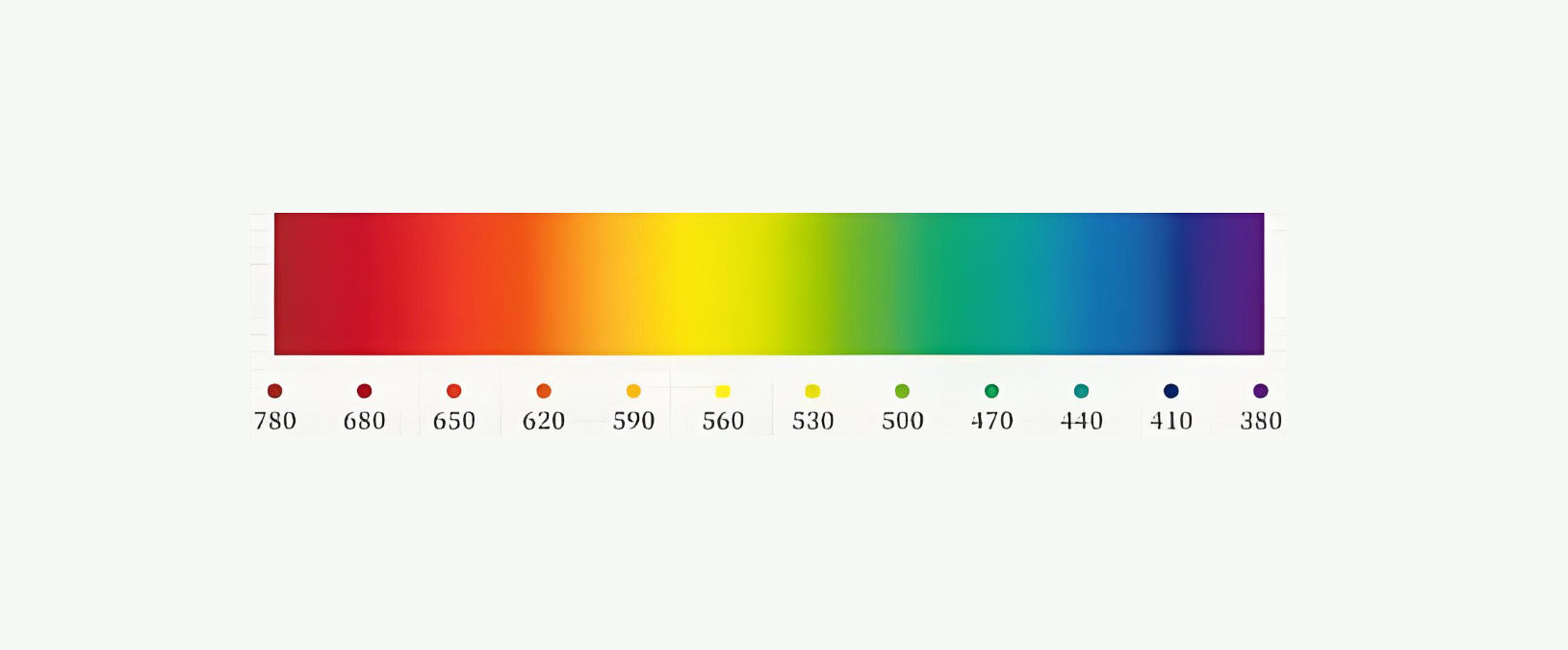
850 nm Near-Infrared Light
Penetrates deeply into cells & increases cellular circulation
635 nm Visible Red Light
Activates mitochondria & promotes ATP production
How LLLT Works
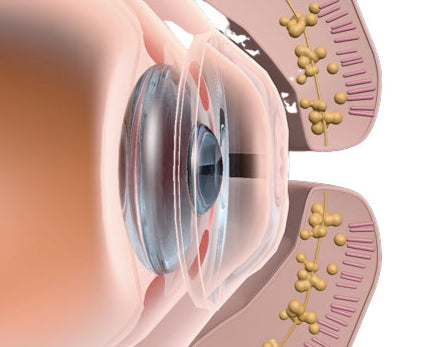
Stimulates Mitochondrial Function
LLLT (Low-Level Light Therapy) stimulates mitochondrial function by using specific wavelengths of light to penetrate cells. This light is absorbed by cytochrome c oxidase in the mitochondria, enhancing the efficiency of oxidative phosphorylation. As a result, the production of adenosine triphosphate (ATP) increases, boosting cellular energy. This process helps improve cell metabolism, repair, and overall function. Additionally, LLLT can reduce oxidative stress and inflammation, contributing to better cellular health.
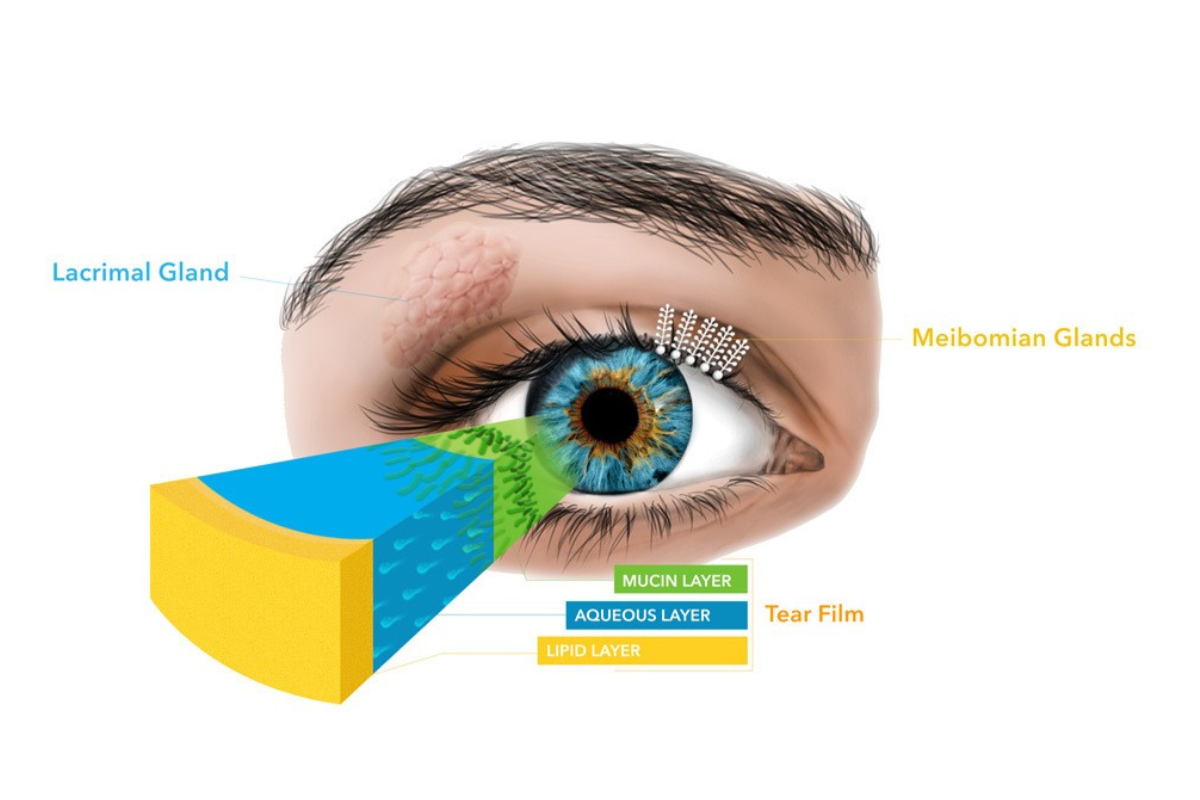
Improves Lipid Secretion
LLLT (Low-Level Light Therapy) improves lipid secretion by stimulating the cells in the Meibomian glands, which are responsible for producing the lipid layer of the tear film. The light enhances cellular metabolism and activity within these glands, promoting healthier and more efficient lipid production. Increased lipid secretion helps stabilize the tear film, reduce evaporation, and alleviate dry eye symptoms, leading to better eye comfort and health.
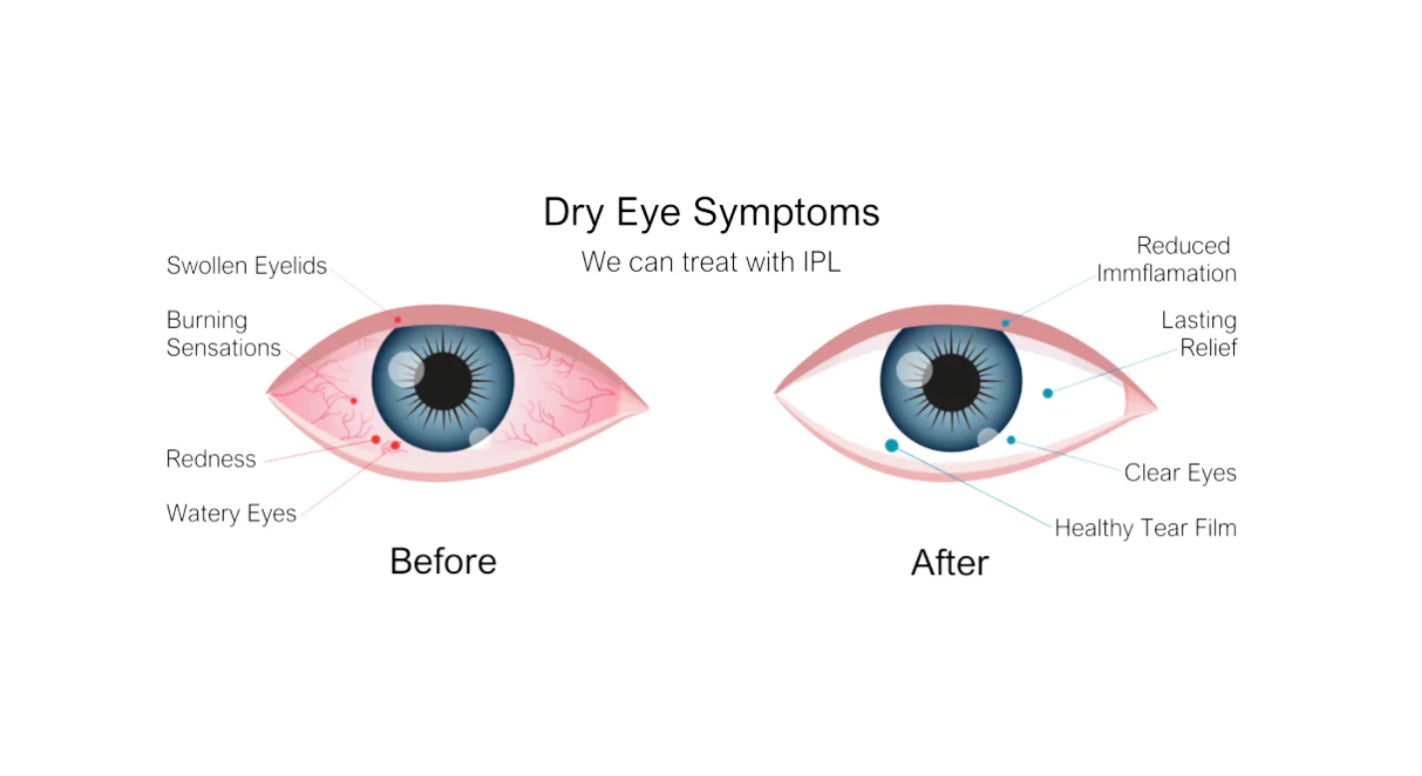
Reduces Inflammation
LLLT (Low-Level Light Therapy) reduces eye inflammation by promoting cellular repair and reducing oxidative stress. The specific wavelengths of light are absorbed by cells, which helps modulate inflammatory responses and decrease the production of pro-inflammatory cytokines. Additionally, LLLT stimulates the release of anti-inflammatory mediators, improves blood flow, and enhances tissue regeneration. These combined effects help reduce inflammation, relieve symptoms, and promote healthier eye tissues.
LLLT (Low-Level Light Therapy) stimulates mitochondrial function by using specific wavelengths of light to penetrate cells. This light is absorbed by cytochrome c oxidase in the mitochondria, enhancing the efficiency of oxidative phosphorylation. As a result, the production of adenosine triphosphate (ATP) increases, boosting cellular energy. This process helps improve cell metabolism, repair, and overall function. Additionally, LLLT can reduce oxidative stress and inflammation, contributing to better cellular health.
LLLT (Low-Level Light Therapy) improves lipid secretion by stimulating the cells in the Meibomian glands, which are responsible for producing the lipid layer of the tear film. The light enhances cellular metabolism and activity within these glands, promoting healthier and more efficient lipid production. Increased lipid secretion helps stabilize the tear film, reduce evaporation, and alleviate dry eye symptoms, leading to better eye comfort and health.
LLLT (Low-Level Light Therapy) reduces eye inflammation by promoting cellular repair and reducing oxidative stress. The specific wavelengths of light are absorbed by cells, which helps modulate inflammatory responses and decrease the production of pro-inflammatory cytokines. Additionally, LLLT stimulates the release of anti-inflammatory mediators, improves blood flow, and enhances tissue regeneration. These combined effects help reduce inflammation, relieve symptoms, and promote healthier eye tissues.
How Does LLLT Treat Dry Eye?
Proven Studies & Clinical Research
This study demonstrates that IPL/LLLT is a safe and effective intervention, yielding a significant and sustained reduction in the symptoms and signs of dry eye disease, with benefits persisting for at least one year post-treatment in a cohort with severe symptomatology. These findings suggest that IPL/LLLT holds promise as a therapeutic option for patients unresponsive to conventional treatments. However, further randomized controlled trials are warranted to elucidate the additional benefits conferred by LLLT.

This study randomized 40 patients (1:1 allocation) to receive either LED low-level light therapy (LLLT group, n = 20) or placebo treatment (placebo group, n = 20). The LLLT group underwent treatment twice weekly for three weeks (6 sessions total). The primary outcome was the change in fluorescein corneal staining (FCS) score, while secondary outcomes included changes in the ocular surface disease index (OSDI), lissamine green conjunctival staining (LGCS), tear film break-up time (TBUT), Schirmer test, and meibomian gland dysfunction (MGD) index. Evaluations were conducted at baseline and 4 weeks post-treatment initiation.
The study demonstrates that one week of consecutive sessions using a newly developed home-based LLLT device significantly enhanced tear film production and stability, alongside alleviating ocular discomfort symptoms in patients with dry eye disease (DED) associated with meibomian gland dysfunction (MGD). These results highlight a promising advancement, offering patients with MGD the potential to benefit from the therapeutic effects of LLLT in a home setting.

This study analyzed 35 eyes from each group treated with either intense pulsed light (IPL) or low-level light therapy (LLLT). Both treatments led to significant reductions in the ocular surface disease index (OSDI) and meibomian gland dysfunction (MGD) severity (p < 0.001), as well as improvements in tear film break-up time (p < 0.001). While both modalities show promise as advanced treatments for MGD-related dry eye, IPL demonstrated superior efficacy compared to LLLT in improving OSDI, non-invasive tear break-up time (NIBUT), and Meiboscore.

The article concludes that combined therapy may induce additional mechanistic benefits, such as enhanced cellular metabolism, alongside greater improvements in symptoms and meibum expressibility compared to LLLT alone. LLLT, however, could serve as an adjunctive treatment option for meibomian gland dysfunction (MGD), particularly in cases where intense pulsed light (IPL) is contraindicated.
This article conclude that PBM has emerged as a promising modality in ophthalmology due to its potential benefits in managing various ocular conditions. For retinal diseases, PBM has shown promise in reducing inflammation, enhancing retinal cell survival, and improving visual function. In treating corneal and anterior segment disorders, PBM accelerates wound healing, alleviates dry eye symptoms, and potentially minimizes complications following refractive surgeries. The non-invasive nature of PBM, along with its ability to modulate inflammatory responses and expedite tissue repair, positions it as a valuable adjunctive therapy in ophthalmic care. Its integration into ophthalmic practice reflects a shift toward minimally invasive, drugfree treatments that can complement traditional therapeutic approaches. As the field of ophthalmology advances toward personalized and precision medicine, PBM’s ability to target specific cellular pathways and enhance treatment outcomes underscores its relevance and potential in modern ophthalmic care.
Photobiomodulation (PBM), or low-level light therapy, uses red or near-infrared light to enhance cell energy, reduce inflammation, and promote healing by stimulating mitochondria, particularly cytochrome c oxidase, to increase ATP production. It supports tissue repair, nerve and brain function, cell protection, and stem cell activity, offering a safe and effective therapy when applied with appropriate parameters.
LLLT appears to have a wide range of applications of use in dermatology, especially in indications where stimulation of healing, reduction of inflammation, reduction of cell death and skin rejuvenation are required. The application of LLLT to disorders of pigmentation may work both ways by producing both repigmentation of vitiligo, and depigmentation of hyperpigmented lesions depending on the dosimetric parameters. The introduction of LED array-based devices has simplified the application to large areas of skin. There is no agreement as yet on several important parameters particularly whether red, NIR, or a combination of both wavelengths is optimal for any particular application. There is a credibility gap that needs to be overcome before LLLT is routinely applied in every dermatologist’s office.